Development of mRNA vaccines has opened a brand-new tool for researchers to use in the fight against HIV.
A new frontier in medical technology
When the COVID-19 outbreak (caused by the virus SARS-CoV-2) began approaching pandemic status, it was clear that science needed to find an efficient, effective, and swift solution to combat it. This was mRNA’s time to shine! But could this increased attention on mRNA mean that it could soon be used for other diseases like HIV?
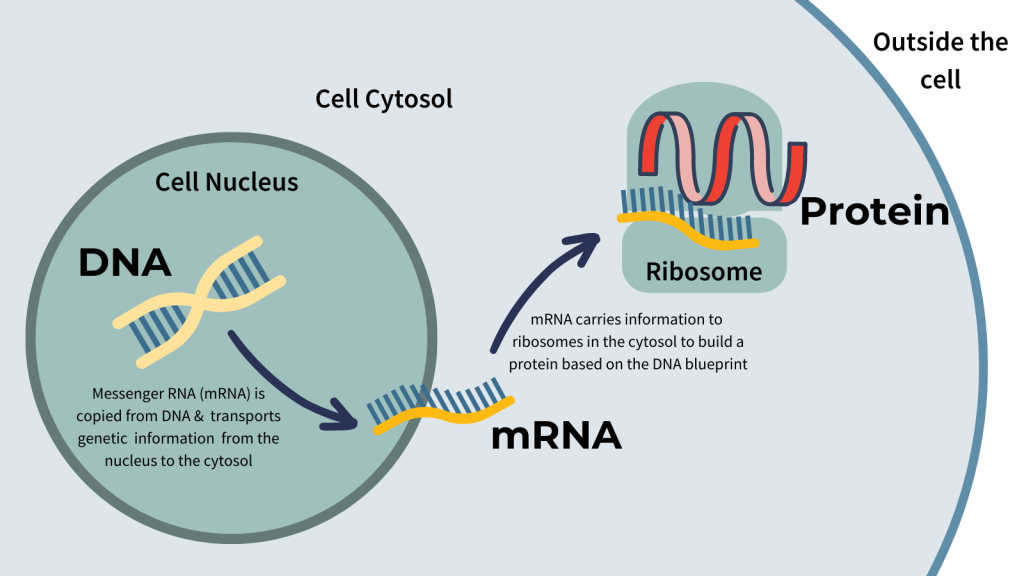
mRNA is a single strand of genetic material used to transfer genetic information from DNA, protected inside the cell nucleus, to the protein-building machinery of the cell, called ribosomes.
Since its discovery in 1964, mRNA has been studied by scientists to better understand how cells function. In the 1980s, scientists figured out how to build mRNA molecules in a lab environment. It was then possible to consider using mRNA as a medical treatment. The first mRNA vaccines in the 1990s were for influenza. The first ever mRNA treatment, for a rare form of blindness, was approved in 2017. Although having mRNA technology as a treatment option has only recently begun, the mRNA molecule itself has been studied for decades. It is an inexpensive, naturally occurring, easily modifiable compound that can be quickly manufactured.
Using mRNA to fight a virus starts with understanding the genetic signature of the virus. This is done with DNA sequencing, which tells scientists how the virus’s genetic material is arranged. Determining the genetic code of COVID-19 helps us understand what it is made of and how it works. DNA sequencing of COVID-19 revealed that spike proteins — molecules that stick out of viruses allowing them to infect other cells — could be a potential target for the immune system and mRNA vaccines. Scientists also found that COVID-19 spike proteins are similar to those of HIV. In fact, COVID-19 and HIV share several similarities. This means that the knowledge gained from understanding and fighting COVID-19 could potentially be applied to beating HIV. It all starts where life begins, at the genetic level.
mRNA & vaccines
DNA is our genetic blueprint, instructing our cells to produce the proteins that make our bodies perform necessary functions for life. All cells throughout the body share the same DNA, but have different functions based on the proteins they build. For example, skin cells make keratin, the protein in hair, and beta cells in the pancreas make insulin. Both these cells have the same DNA, but it would not make sense for beta cells to grow hair or for the skin to make insulin. These cells know which proteins they need to make because of mRNA. mRNA is a messenger molecule that transfers specific instructions from the DNA, safely stored in the cell nucleus, to the protein-building area of the cell. Without interacting with your DNA, mRNA vaccines use this cellular messaging machinery to tell your own cells to make virus proteins so that they can be presented to the immune system in your body. Your immune system then produces antibodies against those proteins, which can detect and destroy similar viral proteins, called antigens, they encounter in the future. It’s possible we can do this for mRNA of HIV proteins.
“It’s like trying to find the Achilles heel of the HIV virus “
CTN Co-Lead of the Vaccines and Immunotherapies Core, Dr. Mario Ostrowski, is an expert on where the HIV virus disarms the immune system. His ultimate goal is to find a cure for the virus. He says that one of the main reasons modern vaccine technologies haven’t worked for HIV is because of the virus’s unique variability.
“HIV is a very diverse virus. Because it mutates so quickly, every person living with HIV has a virus that is unique to them. Its genetic code is constantly changing,” he said.
 HIV mutates thousands of times faster than the COVID-19 virus, SARS-CoV-2. “With a mutation rate so high, we have to think of really new ideas,” said Dr. Ostrowski. “A lot of work is going on to understand how to make a general antibody against HIV so that it can recognize any strain of HIV, regardless of how much it has mutated. This is currently a huge barrier in developing a vaccine against HIV.”
HIV mutates thousands of times faster than the COVID-19 virus, SARS-CoV-2. “With a mutation rate so high, we have to think of really new ideas,” said Dr. Ostrowski. “A lot of work is going on to understand how to make a general antibody against HIV so that it can recognize any strain of HIV, regardless of how much it has mutated. This is currently a huge barrier in developing a vaccine against HIV.”
Because the immune system detects antigens that are on the surface of unwelcome particles, the spike proteins that stick out of viruses are their common target. “HIV has similar spike proteins to SARS-CoV-2, but the mutations of these spike proteins for HIV are even more variable,” explained Dr. Ostrowski. Although mutations occur randomly, because viruses are made up of fewer pieces than other living things, the chance that random mutations affect the spike proteins is high. Random changes within the spike protein can impact how viruses are recognized by the immune system, and by the vaccines designed to support the immune system.
As long as the mutations don’t impact their life cycle, viruses can persist while evading the immune system. Trying to develop a vaccine that covers all the variations of viruses that are present is very challenging. “For example, the Omicron strain of the COVID-19 virus had 50 mutations compared to the original strain,” said Dr. Ostrowski. “Those spike protein mutations only took a few years to develop but they were effective in bypassing the preventative effects of the initial COVID-19 vaccines.”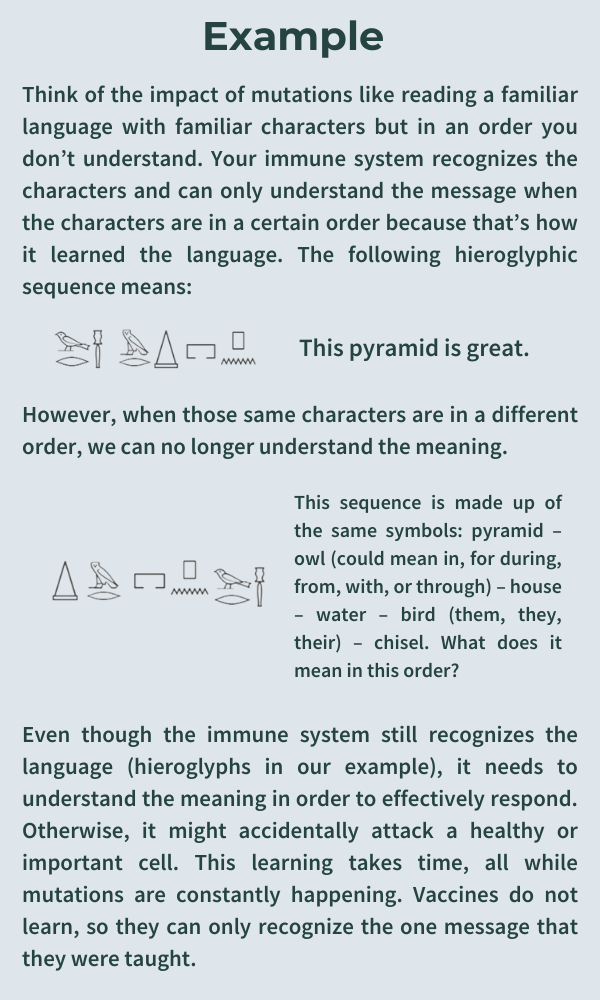
Dr. Ostrowski said that, in someone living with HIV, there may be several mutations of HIV within their body. “That’s the problem with HIV, it does a good job of mutating, so the goal right now is to find an HIV spike protein target that can’t mutate,” he said. “It’s like trying to find the Achilles heel of the virus. Once we know that our target cannot change, we can tailor specific antibodies that could be used in an mRNA vaccine.”
Learning from cancer treatment
Another approach to fighting HIV could be to use mRNA technology to provide treatment tailored to each individual, as opposed to searching for a universal Achilles heel of the virus itself. This is possible because it currently only takes a few weeks to build an mRNA vaccine. Non-mRNA vaccines can take years to develop and test.
Originally, mRNA vaccine research focused on treating advanced cancer. “The beauty of this strategy is that when a person develops cancer, they can also develop an immune response to cancer,” said Dr. Ostrowski. “Because everyone’s cancer is unique, everyone’s immune response to their cancer is unique.”
Genetic technology has allowed scientists to read and understand the genetic sequence of a person’s unique cancer and check to see which part could stimulate an immune response. These foreign parts of the cancer act like antigens. Once they are isolated, these antigens can then be presented to the immune system using mRNA vaccines, allowing the immune system to target the cancer. The goal for cancer-fighting mRNA vaccines is to carry the blueprint of these cancer antigens and see if they can produce a targeted immune response to that cancer. Dr. Ostrowski explains, “The vaccine would essentially enhance a patient’s immune system and help them fight off the cancer. This is called cancer-immunotherapy and is a therapeutic vaccine as opposed to a preventative vaccine, which is what the COVID-19 vaccine was designed to do.”
Theoretically, a therapeutic mRNA vaccine to boost a person’s immune system could be used as a treatment option for people living with HIV. On the other hand, a preventative mRNA vaccine for HIV would be designed specifically to impede HIV’s ability to initially infect a person.
Can mRNA technology treat HIV?
The research community has interest in applying these principles for a personalized therapeutic vaccine against HIV. This is possible because mutations happening within the HIV virus slow down once a person is on antiretroviral therapy (ART). ART prevents HIV from copying itself, which significantly reduces the opportunity for new mutations to occur.

CTN Investigator Dr. Mario Ostrowski
“It would be tailored to the individual,” said Dr. Ostrowski, “So one therapeutic vaccine for HIV would help one person completely eradicate the virus and the infection. It would require obtaining the genetic sequence of each person’s HIV and developing a personalized mRNA vaccine for that person.”
Currently, it is unknown if personalized mRNA vaccines for HIV would work at a population level, but the theoretical potential is there. If a universal Achilles heel is found, then this mRNA technology could apply to a larger population. There are people living with HIV, known as elite controllers, a sub-population of long-term non-progressors, who don’t need medication to remain virally suppressed. Their ability to naturally suppress the virus is sometimes due to genetic features that support an HIV-specific immune response against the infection. The goal of personalized mRNA vaccines is to produce a similar type of strong immune response in everyone living with HIV, not just those who are long-term non-progressive.
“I think mRNA technologies are going to be useful,” said Dr. Ostrowski. “Whether they are going to be completely successful is really still unclear, especially in preventing HIV. They might be more useful in immunotherapy in people who are already living with HIV to see if we can further stimulate their immune systems to get rid of persistent HIV variants.”
Dr. Ostrowski’s laboratory is currently doing feasibility studies to test whether it is possible to bring mRNA technology to people living with HIV to help them eradicate and control their virus using their own immune systems.






